12,079 ViewsThe benefits of IV therapy are vast. They’re not just for athletes and the…
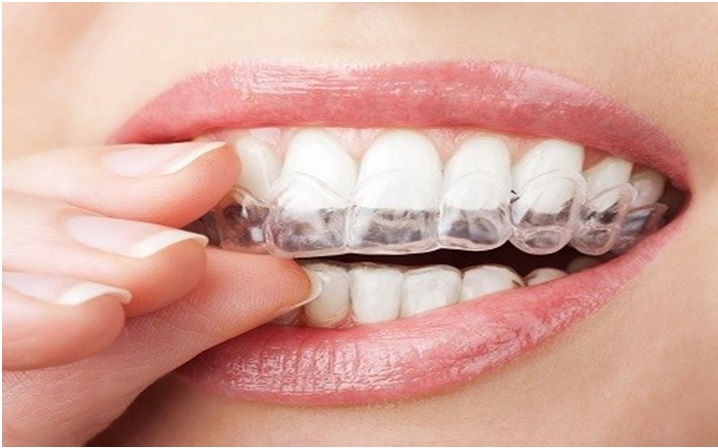
7,992 ViewsIf you are looking to get bright and white teeth, teeth whitening are the…
9,502 ViewsAfter the scorching hot summers, monsoon comes as a relief for not only the…
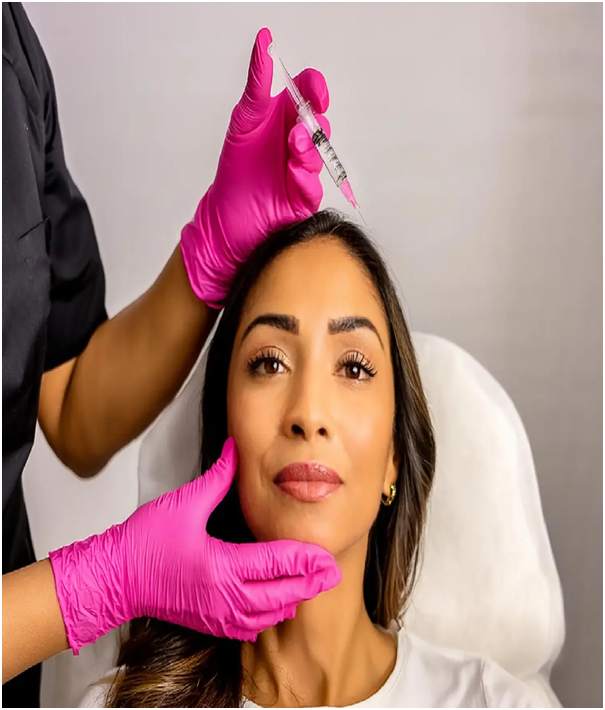
90 ViewsCreating youthful, radiant skin is not simply an issue of genetics. Rather, it’s a…
109 ViewsMelanin rich skin is naturally resilient vibrant and expressive. It has unique strengths such…
160 ViewsHair loss can be more than a cosmetic concern—it can shake your confidence, affect…
376 ViewsAt Victoria Rose Aesthetics Clinic in Pickering, beauty is defined not by dramatic transformations,…
173 ViewsPtosis—commonly referred to as a drooping eyelid—is more than a cosmetic concern. It can…
168 ViewsChoosing the right tooth replacement option is a critical decision for both oral health…
321 ViewsProgress has never been about speed; it’s about sense. We’ve mastered acceleration but forgotten…
269 ViewsBurnout has become one of the defining health challenges of modern life. Whether it…
1,394 ViewsThe benefits of reading every day are many. It impacts diverse aspects of one’s…
723 ViewsSpinach is a leafy vegetable that deserves a place in every kitchen. Whether tossed…